Five Senior Fall Prevention Questions to Ask Your Patients
Falls are the leading cause of injuries in elderly adults, yet it isn’t standard practice for health care providers to ask their patients about accidental falls. With an older adult falling every second of every day, it’s essential to conduct fall risk assessments. Studies show assessment, treatment and follow-up can effectively reduce falls.
There are many factors that can increase fall risk. Assessing fall risk should include at a minimum:
- History of accidental falls
- Impaired gait or mobility
- Visual impairment or dizziness
- Chronic medical conditions such as diabetes, osteoporosis, arthritis or Parkinson’s disease
- Medications associated with elderly falls
- Orthostatic hypotension
- Incontinence
- Altered mental status or cognitive limitations
- Foot problems/pain
- Home fall hazards such as poor lighting, clutter and slippery floors
- Use of assistive devices
- Tethering to IV lines or other equipment
As part of the fall risk assessment process, there are several important questions to ask. “If we don’t ask the right questions, we miss the opportunity to help,” says Ashley Joiner, PT, senior director of regional therapy services for Amedisys Home Health in the Southeast.
Here are five useful and often overlooked questions in fall prevention:
1. Have you had a fall in the past 12 months, or are you afraid you might fall?
Conducting a falls history is a standard part of most fall risk assessments. Patients are more likely to fall if they have fallen in the past year. Once an older adult has a fall, they often become overly cautious and restrict their activities, which creates a cycle of increased fall risk. Even if they have not fallen in the past, a fear of falling can lead to inactivity and balance problems that increase the risk of falling.
With less than half of older adults telling their doctor if they fall, it’s important for health care providers to proactively address fall prevention.
“Fall risk should be routinely assessed with steps taken toward prevention, the same way as heart disease and stroke,” says Joiner. “Statistics don’t capture the large number of people who have falls that exacerbate something else, and that something else ultimately leads to their demise.”
If an older adult says they have fallen in the past year, it’s important to follow up with questions about:
- The number of accidental falls
- Circumstances surrounding the fall
- Premonitory symptoms
- Ability to get up after an elderly fall
- Any injuries sustained
- Any medical treatment received
- Fear of falling again
[action 1]
2. Have you had any loss of balance where you stumble or trip, even if you don’t fall down or get injured?
Many older adults think of an accidental fall as a life-changing event that causes injury. When asked if they’ve fallen or are afraid of falling, many underestimate their risk. They may not recognize that a near-fall is an important indicator of their level of functioning and that they can take steps to mitigate their fall risk.
“A fall is defined as coming to rest on a lower level,” notes Michelle Lusardi, PT, DPT, PhD, FAPTA, a geriatric fall expert and professor emeritus at Sacred Heart University. “Often older adults don’t realize they don’t have to go all the way down to the floor for it to be considered a fall.”
“It isn’t enough to ask if the patient has had a fall,” says Joiner. “Many older adults will say they haven’t fallen because they didn’t tumble down the stairs and get injured. But they may have tripped over the dog or fallen into a wall and caught themselves. We have to get more specific because they don’t realize it’s an issue for them.”
Asking questions and listening attentively are just part of fall prevention. “We have to observe using all five senses, not just what is being told to us,” Joiner adds. For example, how does the patient get up from the table? Talking to their family member or caregiver can also produce valuable insights.
3. Have you stopped doing things you enjoy?
Many older adults don’t realize they’ve changed their routine to accommodate their fear of falling. “As people age, they often stop doing things they love, even basic activities of daily living,” says Luzelle Havenga, Amedisys’ assistant vice president of therapy innovation. “They need to be asked, ‘Why did you stop?’ For many, it boils down to fear of falling, which can be addressed so they can enjoy life again.”
Another way to ask the question, says Lusardi, is “Are you as active as you were six months ago?” “Sitting down may feel like a good way to prevent falls,” she says. “But balance is a practice-makes-perfect system – it gets less efficient the less you use it. In the long run, not moving is riskier than moving.”
4. What do you want to be able to accomplish?
It’s important for health care providers to prioritize each patient’s specific wants and needs. “There’s an assumption that when you get old, you fall. This doesn’t have to be the case,” says Melanie Wortman, the senior director of regional therapy services at Amedisys Home Health. “People are quick to limit older adults’ lives because it’s easier to tell them to always use a walker or avoid certain activities. What we need to ask is, ‘What do you want to be able to do?’ and set up a program to get them there.”
When Wortman’s grandmother fell and ended up with a fracture in her spine, it was important to her to be able to continue cultural practices that involved kneeling and getting down on the floor. The question for her caregivers wasn’t whether she should do those things, but rather finding the safest way to allow her to live the life she wanted.
Lusardi goes one step further and believes older adults should regularly practice getting up and down from the floor. One of her first physical therapy patients fell from her chair at her desk and got stuck, but because of her movement practice was able to scoot herself into the living room and get up using the couch. Six months later, she was outside tending to her rose garden.
5. What medications are you currently taking?
Medication review is a critical part of a fall risk assessment. Certain medications, such as blood pressure drugs, sedatives, antidepressants, antipsychotics and some pain relievers, can increase the risk of falls. If an older adult takes four or more medications a day, the side effects also can increase their fall risk. In some cases, lower doses or alternative medications may be necessary.
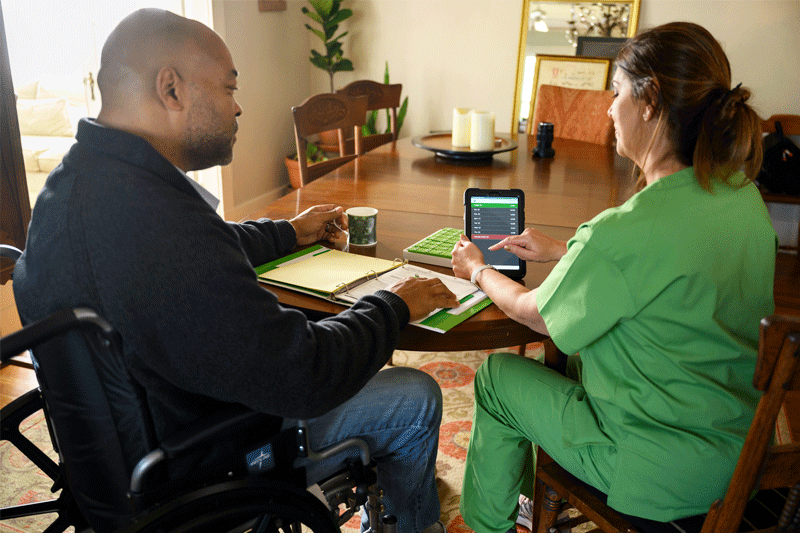
How Home Health Care Can Help Prevent Falls
Researchers have found that healthcare providers can help reduce elderly falls by referring older adults to specialists such as occupational therapists for home modification and physical therapists to treat balance and mobility problems. In fact, home modification by an occupational therapist was the most effective clinical fall intervention compared to six other interventions studied.
Home health care is a valuable resource that can help with several evidence-based fall prevention strategies including:
- Balance and strength exercises with a physical therapist
- Environmental assessment and modification by an occupational therapist for safe functioning at home
- Management of medications and chronic medical conditions with skilled nursing
- Speech therapy to improve cognition, nutrition and hydration
- Social work for counseling and support
- Assistance with activities of daily living from home health aides
“We’re right there in the home with patients, so we can look at falls from a holistic perspective,” says Joiner. “From this unique vantage point, we can be the whole medical team’s eyes and ears.”