As you age, the community – and even your own home – can feel like a minefield. From rugs and wet floors to stairs and uneven sidewalks, obstacles are everywhere.
The fear of falling is understandable. One out of four people age 65 and older falls each year. “You may have fallen in the past and don’t want it to happen again,” says Melanie Wortman, the senior director of regional therapy services at Amedisys Home Health. “Fear of falling can also be based on experiences friends and family have had.”
LEARN ABOUT AMEDISYS' FALL REDUCTION PROGRAM
For older adults, fear of falling outranks other common concerns such as financial fears and getting robbed. Elderly falls can affect your health and quality of life. Accidental falls can cause bruises and soreness. They can also be more serious. One in five falls causes broken bones or a head injury. As the leading cause of injuries in elderly adults, falls can lead to disability and expensive trips to the hospital.
“I believe it’s underreported how much a fall can affect an older adult,” says Ashley Joiner, PT, senior director of regional therapy services for Amedisys in the Southeast. “You hear about people passing away from heart disease and cancer but not falls or disease processes that are intensified from a fall. Even if falls aren’t the direct cause of death, they often make symptoms worse and exacerbate something else that causes a faster decline.”
Much to Fear, Including Fear Itself
While fear of falling is understandable, the fear itself makes you more likely to tumble. You may feel paranoid about leaving the house. Or you could be afraid to take a shower, clean the house or do much of anything. Fear stops you from living.
Here are a few ways fear of falling makes you more likely to fall:
- Inactivity – Fear of falling stops older adults from staying active. The less you move, the less you’re able to do daily activities like bathing and shopping. Physical weakness, in turn, increases your risk of falling.
- Balance – The fear in your mind can translate into changes in your body. You take steps to try to prevent falling, such as walking slower and widening your stance. These changes can throw off your balance, which increases the risk of falls.
- Mental health issues – Staying inactive at home can cause symptoms of depression and anxiety. The medications used to treat these mental health issues may make you more likely to fall. If you use alcohol or other drugs to cope, your fall risk is even higher.
“When you’re afraid of something, the fear can take over and destroy your confidence,” says Joiner. “What we often see is that people nestle themselves into a 6’ x 6’ box in their home so they don’t have to move. They call themselves independent but their quality of life is horrible. Movement truly is medicine to combat this vicious cycle.”
Many older adults don’t realize they have a fear of falling. When Joiner’s grandmother fell in the bathroom, she never acknowledged that she was afraid of falling or that she had changed her behavior because of her fall. “But as family members, we noticed,” Joiner says. “There were posture changes. She wore different clothes that were easier to put on. She did more ‘furniture walking’ and ate dinner on the couch rather than at the dinner table. It was a total change in everything she did that was never verbalized or acknowledged. Had we dug deeper, we would’ve realized it was all out of fear of falling.”
[action 1]
Risk Factors for Falls
What causes falls in elderly adults? Several factors can increase your fall risk:
- Having a previous fall
- Pain in your lower body, which can change your posture and how you move
- Low vitamin D levels
- Poor balance
- Weakness in your lower body
- Difficulty walking
- Use of prescription or over-the-counter medications that affect your balance (such as sedatives or tranquilizers)
- Poor vision or hearing
- Foot pain or unsupportive shoes
- Fall hazards in your home such as clutter, uneven steps or throw rugs
How many risk factors for falls do you have? The more you have, the greater your risk of falling. The good news is you have the power to change many of these risk factors and prevent falls.
Fall Prevention Tips
No one can tell you, “Don’t be afraid.” The fear is valid and real. But there are steps you can take to manage your fear so it doesn’t cost you your independence:
Talk about your fear. Sharing how you feel may help you work through your fears. It also educates your family and caregivers so they can give you the best care. Less than half of older adults tell their doctor if they fall. Be sure to tell yours. If you do, they can help by:
- Providing a fall risk assessment to understand your risk for a fall
- Reviewing your medications to make sure they aren’t increasing your fall risk
- Referring you to physical therapists, occupational therapists and home health care agencies that can help keep you active and safe
- Recommending a cane or walker, if needed
- Signing off on an exercise plan
- Recommending vitamin D supplements, if needed
If your doctor establishes your eligibility for the Medicare Home Health Benefit, you may have access to home health care services that can help prevent falls. This could include:
- Skilled nursing to manage medications and chronic conditions
- Occupational therapy to assess home fall hazards
- Physical therapy to improve balance, posture, strength and coordination
- Speech therapy to improve cognition, nutrition and hydration
- A home health aide to monitor and assess the safety of the home environment
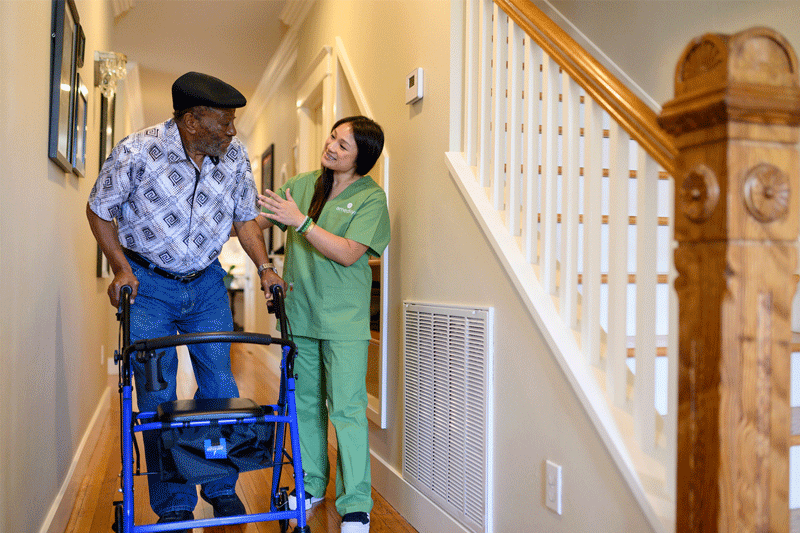
“Our greatest strength is that we’re in patients’ homes,” says Joiner. “We see how they’re functioning in their own environment so we can be the whole medical team’s eyes and ears. Most falls happen in the home, so what better place to address them than right there in the home with them?”
Check your vision. The Centers for Disease Control and Prevention recommends getting your eyes checked once a year.
Take appropriate precautions. You’ll feel more confident if you take steps to protect yourself. There are products that may lower your fall risk such as dressing sticks and elongated shoehorns. An occupational therapist can help you identify products that can help you in the home. You can also work with a physical therapist to strengthen your muscles and improve your balance and posture so you can walk smoothly.
Make your home safer. More than 75% of falls happen in or around the home. Home health care agencies can modify your home to make it safer. In one study, researchers found that home modification by an occupational therapist was the most effective clinical fall intervention compared to six other interventions they studied. For example, an occupational therapist might:
- Move fall hazards such as rugs, clutter or other things you could trip over
- Add grab bars near your toilet and shower/bathtub
- Add railings to the stairs
- Add lights or change lightbulbs to make sure you get enough light
Keep moving. Like all good things in life, healthy aging takes work. If your doctor recommends it, try exercises such as tai chi and yoga. These forms of gentle movement focus on building balance and leg strength so you can get up and down easily. Even if you have family help or a home health aide, do basic chores around the house if you’re able. Everyday activities like folding laundry, cleaning and gardening can help keep you moving.
“Giving people personalized tools to stay active and be successful long-term is magic for our patients,” says Luzelle Havenga, Amedisys’ assistant vice president of therapy innovation. “It totally changes their lives to go from sedentary to enjoying life again.”
Falling doesn’t have to be part of aging. If you’re afraid of falling, talk to your doctor. There are steps you can take to rebuild your confidence and preserve your independence.